COVID-19 Best Practices for the Shipowner
[Dr. Arthur L. Diskin, M.D., global medical director of maritime medical services firm Future Care, publishes regular bulletins on the latest clinical research and best practices related to COVID-19 control for shipping. His latest guidance appears here in an abbreviated form.]
Reducing infection and transmission
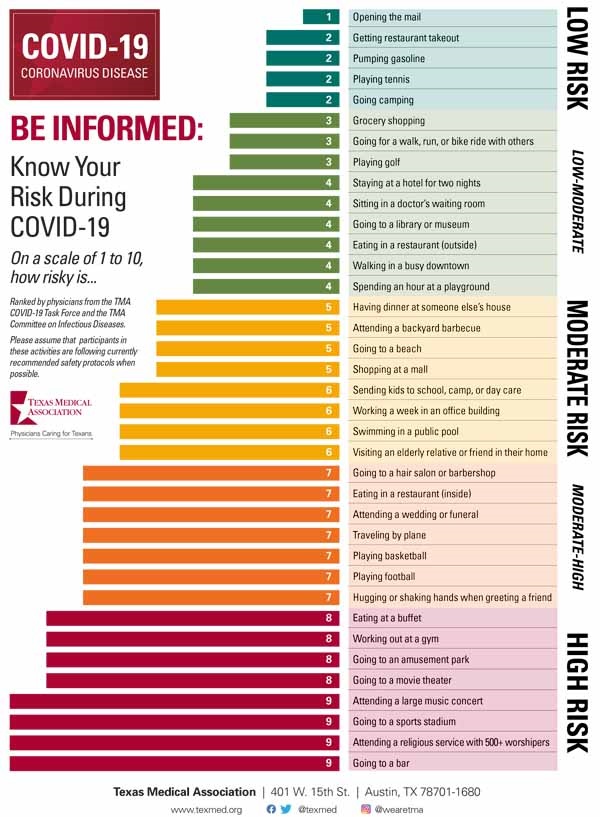
The Texas Medical Association recently came out with an excellent relative risk chart for a variety of different activities. Some shipowners have asked about permitting shore leave. Perhaps if you were required to provide shore leave, you could require that no one participate in activities above level four?
In addition, this chart from the New England Journal of Medicine is an excellent reference point as to required activities that can truly limit transmission and spread.
Airborne Transmission
We must begin to address the realities of airborne spread – not only for this virus but for future pathogens. COVID 19 virus particle size is 125 nanometers (0.125 microns); the range is 0.06 microns to 0.14 microns. However, the viruses are carried on droplets (>10 microns) and aerosolized particles (< 5 microns). Exact definitions vary as to what particle size is a droplet vs aerosolized. However, a small droplet can evaporate enough water content to become an aerosolized particle.
In general, infected people spread viral particles whenever they talk, breathe, cough, or sneeze. Such viral particles are known to be encapsulated in particles of mucus, saliva, and water, and the fate/behavior of these particles in the environment depends on the size of the particles. Bigger particles fall faster than they evaporate so that they splash down nearby in the form of droplets. Smaller droplets evaporate faster and form aerosols and bioaerosols, linger in the air, and drift farther away than the larger droplets do.
Viral disease outbreaks via aerosol transmission are not as severe as one would think, because of dilution and inactivation of viruses that are suspended for extended periods in the air. Ventilation currents, temperature and humidity may all effect the presence of aerosolized viral particles. It is still considered that droplet transmission and surface to mouth transmission are the two major routes of transmission.
Droplet transmission is best limited by facemasks – all parties at all times when face-to-face contact is possible, with or without social distancing adherence. Excellent and validated sanitation practices along with frequent hand-washing and/or use of hand sanitizers is key for prevention of transmission from direct contact with infected people or contaminated surfaces.
However, the transmission of the virus by airborne transmission -especially in situations where the virus can hang indoors in a crowded environment with low air flow - needs to be considered.
Inhaling small airborne droplets is now considered probable as a third route of infection. There is a significant body of evidence for other respiratory viruses being transmitted in this manner to varying degrees, and therefore SARS-CoV-2 should not be treated any differently – at least having the potential for airborne transmission indoors.
How to impact potential aerosolized transmission
The CDC has a pyramid of control for pandemic pathogens, below:
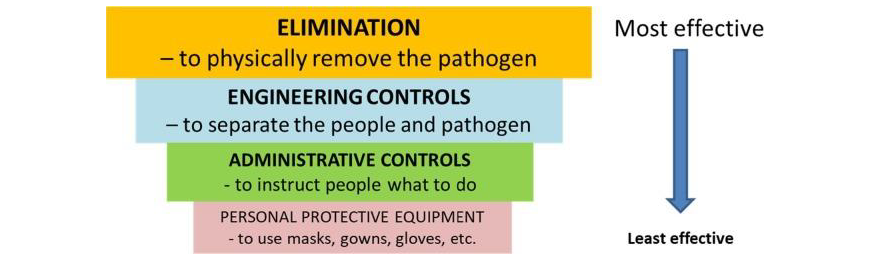
Traditional infection control pyramid adapted from the US Centers for Disease Control
Engineering controls are critical to the avoidance of airborne spread. In order to limit the exposure, there must be appropriate environmental and building (or ship) engineering controls in place. General recommendations must be made specific to the facility.
• Sufficient and effective ventilation: In most buildings ventilation rates are much lower than hospitals to save energy and costs. HVAC systems are complex and specifically designed for a given building or vessel according to specific parameters including control of temperature, relative humidity, air flow distribution and direction. The HVAC engineers must be involved in any decisions and ASHRAE (The American Society of Heating, Refrigerating, and Air-conditioning Engineers), REHVA, SHASE (The Society of Heating, Air-Conditioning and Sanitary Engineers of Japan) have all updated their guidelines to address the spread of COVID-19. Whenever possible, natural outside air should be part of the ventilation plan, even if that air needs to be filtered of pollutants or heating must be increased in winter.
• UV disinfection: Enhanced by particle filtration and air disinfection, UV-C light can most likely inactivate the virus. One strategy that is very effective and at least as good as doubling the ventilation rate in the right room is ‘upper-room’ UV system. UV lamps are placed in the upper part of the room, wall or ceiling mounted, and directed to the “upper zone” limiting UV exposure in the occupied space below. This works even better with fans increasing circulation.
• Avoidance of air recirculation: The recirculation of air should be avoided wherever and whenever possible and when unavoidable there should be UV light (or appropriate filtering) within the recirculation system Recirculation may be used to save money but can result in the transport of airborne contaminants (including infectious viruses) from one area to another increasing the risk of airborne infection in areas that otherwise would not have been contaminated. Large central units should be operated on 100 percent outside air whenever possible. Filters and disinfection units can be placed in the recirculated streams but need to be well-designed, properly located and serviced regularly. They must also be tested and rated for particle size to insure filtering of pathogens or effectiveness in destruction of viral particles.
• Avoiding overcrowding: This is self-explanatory. Increased person density can overwhelm the ventilation and airflow strategies very quickly. An option in any space is to use a surrogate for suspended virus such as particle or VOC concentrations and utilize sensors to feedback to the HVAC system increasing flow rates.
Improving air flow should always start with improving outside ambient air flow. In certain environments this may require filtering of pollution. At other times, opening windows in very hot or cold climates might require increased output from heating or cooling elements. Indoor and centralized ventilation systems should use outside air to the highest degree possible minimizing recirculation. If recirculated air is necessary, then there should be something in the outflow track such as gUV lights or dry hydrogen peroxide units.
Lastly, design all working areas with decreased density and appropriate social distancing tools.
PCR testing
Good data on the sensitivity and specificity of the PCR test are lacking due to the absence of an accepted gold standard. Clinical sensitivity varies depending on many factors, including how and when the specimen was acquired, viral load, and the design of the PCR assay. Some papers suggest that initial sensitivity could be about 75 percent. A true nasopharyngeal specimen is collected from the posterior nasopharynx and is generally uncomfortable for the patient, but this likely provides the highest sensitivinty.
All of this suggests that a single negative PCR test may inadequate to rule out COVID-19. The incidence of infection is likely much higher than currently reported.
Saliva testing
The current saliva testing is actually just a collection alternative to the uncomfortable nasopharyngeal swab. The specimen is collected and then needs to be sent to a lab, often the same lab as nasopharyngeal swabs. Ships would need to collect the saliva in the kit and get it to the lab that provided the kit. It should have the same turnaround once it reaches the lab - 12 hours to one week - depending on location and volume of tests, unless you mail it to a specific lab. The specificity should be as good as nasopharyngeal. The sensitivity may be a little bit lower.
Nasal swabs are inherently less sensitive than nasopharyngeal and saliva testing is probably better for home collection kits that are sent to the lab.
Antigen testing
The next step we will see as antigen testing. This is a lot faster and will not be subject to many of the shortages we are seeing in the PCR testing. It is less sensitive. We are substituting speed, cost and convenience for some accuracy and the knowledge we will have a few more false negatives. The accuracy of this modality will continue to improve to the point where there is eventually qualitative testing available at the site. These tests, when they become available, will be exactly what our ships will want to want to carry.
We are at least months if not a year away from this, even with everything moving at lightning speed. When home test kits emerge that allow true collection and testing at home, it will be very important they are of high sensitivity as the implications of a false negative test in someone who is shedding virus is too high. If these tests are being used for screening of workers and the sensitivity is not very high, it is likely they will recommend testing two to three times per week rather than weekly.
Post-exposure testing
The best practice is probably waiting four days after potential exposure to infected individual and get a nasopharyngeal swab test and if the test is negative, repeating five days later. Alternatively, self quarantine, wait 14 days after exposure and if there are no symptoms then the quarantine is done. We may see this recommendation dropped from 14 to 10 days soon.
Antibody testing: The US Food and Drug Administration (FDA) has revoked the emergency use authorization (EUA) for one of the first antibody tests authorized during the COVID-19 public health emergency. We must be very cautious with our use and interpretation of antibody tests. Antibody testing is not recommended for the diagnosis of acute symptomatic infection as a stand alone test. It is also not recommended for asymptomatic patients trying to rule out acute infection.
When can my employee go back to work?
The recommendations for testing for back to work are a moving target because it has become evident that many people continue to test positive or even test negative and then positive again. Studies have shown that this does not correlate with live virus or viral transmission. Recall that RT-PCR does not measure live virus, it indicates the presence of viral antigens.
There is some correlation with sicker individuals shedding virus for longer periods of time. Our back to work recommendations should take this into account. Individuals who were sick enough to be hospitalized should have their back to work dates determined by their treating physicians and should be recommended to wear a mask upon return to work - indefinitely preferred, but to a minimum of 20 days after the positive test or start of symptoms - whichever is later. For individuals with minor symptoms or asymptomatic, the performance of testing to clear them for return to work is only confusing.
Phases and treatment of COVID-19
We have clearly observed that illness associated with SARS-CoV-2 infections seems to have two phases. In the first phase, viral replication causes mild to moderate symptoms, and the severity of infection can be reduced by reducing the replication of the virus. In the second phase, symptoms and damage to the body are due to an extreme response of the immune system many have named cytokine storm, which can be countered by use of anti-inflammatory medications.
Anti-inflammatory medications can also reduce the body’s natural immune response to the virus, which is less of a concern later in COVID-19 because viral replication is less important. However, use of anti-inflammatory medications can disrupt the initial immune response to the infection and lead to worse outcomes when taken early for COVID-19.
What this means is that studies are not only addressing what medications to give but when to give them. Recent studies with hydroxychloroquine have shown it may be effective when given earlier in the course of disease than previous studies that showed no effect.
Other treatments
Steroids, such as dexamethasone, have been shown to either not work or have negative responses when given too early or with minor symptoms before the overactive immune response has started. Timing will be critical.
Dexamethasone, the familiar glucocorticoid, reduced deaths in hospitalized COVID-19 patients with severe disease by one-third compared to those receiving usual care, according to interim results from the RECOVERY trial recently released.
Remdesivir continues to be the mainstay of clinical treatment in severely ill patients meeting specific criteria. It appears to improve mortality, decrease time on the ventilator and decrease hospital stay. It helps but is far from a cure.
Tocilizumab is an antibody medication that targets interleukin-6 (IL-6), which is one of the cytokines that is involved in the over-activation of the immune response with severe cases of COVID-19. It is currently only given to critically ill patients already in the second phase of the illness.
Acalabrutinib, a Bruton tyrosine kinase (BTK) inhibitor, showed early signs it may improve outcomes quickly for patients with severe COVID-19, a case study of 19 patients has found.
There are also ongoing studies of antibodies to prevent infection. There are at least two drugs in human trials called monoclonal antibodies, which are created by using immune cells. The two treatments block the spike protein on the coronavirus that allows it to enter human cells - one of them uses 2 different antibodies against 2 different proteins.
Additionally, there are specific syndromes that certain patients get such as stroke or pulmonary embolism that need specific treatment.
Vaccine Development
There are more than 60 candidate vaccines currently in development, according to the World Health Organization. Many are in preclinical stages and some are beginning clinical trials. The world has now witnessed the compression of six years of work into six months on these vaccines, so where we are is very impressive but still a long way to to go. Current methodologies and prior knowledge about spike proteins on coronaviruses have helped.
The challenge is create a vaccine that is both safe and effective – both in healthy individuals and those older or immunocompromised. You also have to make sure the vaccine does not make someone who is sick or has been exposed to the virus worse (immunopotentiation). The immune functions that decline with age and that are likely to be responsible for the greater risk of severe Covid-19 in older adults may also lead to poor vaccine responses.
Additional time for production and distribution will be required after development.
Vaccine strategies
There are a wide variety of strategies to design a vaccine. Moderna is attempting a vaccine based on mRNA causing the body to produce the antigen. Vaxart is attempting to develop an oral vaccine. Vaccines at Oxford in England and China using weakened adenovirus to deliver a gene encoding SARS-CoV-2 antigen, so the body will recognize the antigen when exposed are both showing a high degree of promising early results.
My best guess is that there will be one or more vaccines available for healthcare workers and high risk individuals in the first quarter of 2021 and for the general population by mid-2021. Maybe I will be pleasantly surprised with an earlier vaccine.

that matters most
Get the latest maritime news delivered to your inbox daily.
However, in order for the vaccine to work, people must take it. In at least one survey only 40-50 percent of the surveyed population said they would take the vaccine.
Arthur L. Diskin, M.D., FACEP is Global Medical Director of Future Care, Inc.
The opinions expressed herein are the author's and not necessarily those of The Maritime Executive.
